Abstract

Introduction:
Follicular lymphoma (FL) is characterized by an indolent clinical course, but patients with this disease bear a risk of transformation to diffuse large B-cell lymphoma (DLBCL) or high-grade B-cell lymphoma (HGBL). DLBCL transformed from FL (tDLBCL) traditionally has been associated with an aggressive course and a post-transformation survival of 0.6-1.7 years. However, a more recent study showed longer survivals in these patients, challenging the notion that transformation universally portends a poor prognosis in the immunotherapy era. Presence of concurrent FL at the time of diagnosis of DLBCL (cDLBCL/FL) also raises the possibility of transformation, but its clinical significance has not been elucidated in the literature. In this study, we analyzed and compared outcomes of tDLBCL, cDLBCL/FL, and de novo DLBCL. We also characterized the prevalence of MYC/BCL2/BCL6 gene rearrangements in tDLBCL and cDLBCL/FL cohorts and evaluated the impact of dual rearrangements (double hit, DH) on clinical outcomes.
Methods:
Patients diagnosed with DLBCL or B cell lymphoma unclassifiable with features intermediate between DLBCL and Burkitt lymphoma, also known as HGBL (BCLU/HGBL), treated at Northwestern University or University of Pennsylvania from 1/2010 to 7/2016 were included. Patients with Burkitt lymphoma, primary CNS and HIV-associated lymphoma were excluded. Transformation was defined as presence of DLBCL/ BCLU/HGBL in cases with an antecedent diagnosis of FL by at least 6 months. We divided our cohort into three groups: 1. De novo DLBCL or BCLU/HGBL with no prior history of FL (dDLBCL) 2. Transformed FL (tDLBCL) and 3. DLBCL or BCLU/HGBL with concurrent FL (cDLBCL/FL). Progression free survival (PFS) was defined as time from diagnosis to radiographic progression, regimen change, death or last follow-up. Overall survival (OS) was defined as time from diagnosis to death or last follow-up. Kaplan-Meier (KM) survival analyses, using a log-rank p-values were performed for PFS and OS to compare the three diagnosis groups (dDLBCL, tDLBCL, and cDLBCL; alpha=0.05) and pairwise comparisons of combinations of diagnosis (dDLBCL and tDLBCL+cDLBCL) and double hit status (accounting for multiple comparisons with a Bonferroni corrected alpha=0.013). Fluorescence in situ hybridization for MYC, BCL2 and BCL6 rearrangements was performed using break-apart probes per the policy of each institution.
Results:
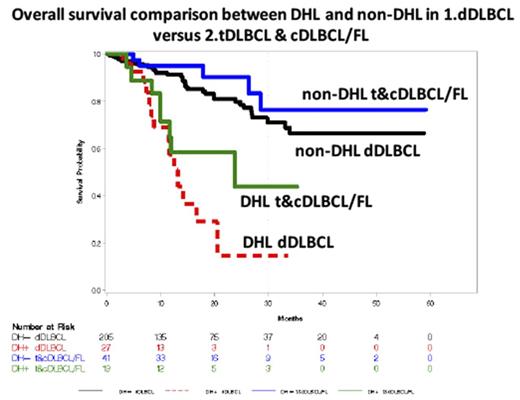
A total of 293 pts, including 233 dDLBCL, 37 tDLBCL, and 23 cDLBCL/FL were included. 50% of the tDLBCL received at cytotoxic chemotherapy before transformation for precedent FL. Age and sex distribution, as well as clinical characteristics including stage, ECOG performance status, IPI score, and primary refractoriness were similar amongst the three groups. LDH was more likely to be elevated in dDLBCL (75%), as compared to tDLBCL(63%) and cDLBCL/FL (47%)( p=0.02%). Additionally, non-bone marrow extra-nodal disease was seen more often in dDLBCL (72%), as compared with tDLBCL (53%) and cDLBCL/FL (43%)( p <0.01). DH were seen more often in tDLBCL(32%) and cDLBCL/FL (30%), compared with the dDLBCL (11%)( p <0.01). The cell of origin was germinal-center type in 92% of the tDLBCL and 91% cDLBCL/FL, compared with 64% of dDLBCL (p <0.01). Intensive chemotherapy regimens (R-EPOCH or R-hyperCVAD) and autologous stem cell transplantation was used more often in tDLBCL (43% and 19%, respectively), compared with dDLBCL (30% and 3%, respectively) and cDLBCL/FL (28% and 8% respectively). For all pts, the median length of follow-up was 13.8 months (range 0.2-59.2). OS and PFS were similar in the three subgroups (p=0.90 and p=0.77, respectively; Figure 1). We then analyzed the survival based on the presence of DH in two separate subgroups: 1) dDLBCL and 2) tDLBCL + cDLBCL/FL (combined as one group given low number of cases). OS was significantly shorter in lymphomas with DH, compared to non-DH in both subgroups (p <0.001 for dDLBCL and p=0.004 for tDLBCL + cDLBCL/FL). Comparison of the OS in DH of dDLBCL versus DH of tDLBCL + cDLBCL/FL showed no statistical difference (p=0.15), similar to the OS of non-DH cases the two groups( p=0.31).
Conclusions:
DLBCLs transformed from FL or with concurrent diagnosis of FL (composite lymphoma) demonstrated similar clinical outcomes in our study. However, dual rearrangements are more prevalent in these patients and drive inferior survival similar to DH status in de novo DLBCL.
Landsburg: Curis: Consultancy, Research Funding; Takeda: Research Funding. Winter: Merck: Research Funding; Glaxo-Smith-Kline: Research Funding. Pro: Seattle Genetics: Consultancy; Takeda: Consultancy, Research Funding; Celgene: Consultancy, Research Funding. Gordon: Janssen: Other: Data Monitoring Committee. Karmali: Celgene: Speakers Bureau. Kaplan: Millennium: Research Funding; Takeda: Research Funding; Seattle Genetics: Research Funding; Janssen: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal